At UNTAG, we believe in keeping our knowledge up-to-date and sharing valuable information with our community. That’s why we’ve reviewed recent scientific studies on chest binding. We’ve summarized the key findings and practical tips to help you bind safely and effectively. Chest binding plays a vital role in reducing gender dysphoria and supporting the gender identity of many transmasculine and gender-diverse individuals. However, it’s just as important to be informed about the potential physical health risks and learn how to practice chest binding in a way that is as safe and sustainable as possible.
What Is Chest Binding?
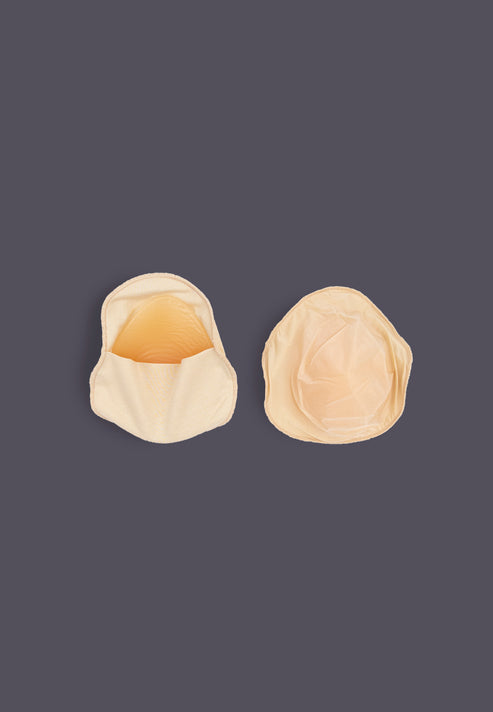
To clarify what chest binding entails, this is a commonly accepted definition: chest binding involves compressing chest tissue to create a flatter chest appearance. It is often used as a temporary alternative to top surgery (mastectomy) or for those who may not have access to or desire surgery. Common binding methods include commercial binders, sports bras, and layered clothing (Peitzmeier et al., 2017).
Health Benefits of Binding
Studies consistently highlight the psychological importance of binding:
- Reduced dysphoria: Binding alleviates the distress associated with a chest that does not align with one’s gender identity (Santos et al., 2022).
- Improved mental health: Participants in multiple studies reported reduced anxiety and depression, increased confidence, and greater comfort in public spaces (Jarrett et al., 2018).
Common Health Risks
However, prolonged or improper binding can lead to health complications. According to Peitzmeier et al. (2017) and Santos et al. (2022), the most common issues include:
- Respiratory problems: Shortness of breath and difficulty breathing are frequently reported (Santos et al., 2022).
- Pain: Back, shoulder, and chest pain are common, with a prevalence as high as 53.8% for back pain (Peitzmeier et al., 2017).
- Skin irritation: Binding can cause itchiness, rashes, and skin infections (Jarrett et al., 2018).
- Postural issues: Bad posture and musculoskeletal complaints, such as rib or spine changes, are also concerns (Peitzmeier et al., 2017).
Factors Increasing Risk
Several factors contribute to the likelihood of experiencing negative symptoms:
- Frequency: Binding daily significantly increases risks (Peitzmeier et al., 2017).
- Duration: Using a binder for extended periods (e.g., more than 8 hours a day) can exacerbate symptoms (Santos et al., 2022).
- Improper methods: Elastic bandages, duct tape, and plastic wrap are linked to higher rates of complications and should be avoided (Peitzmeier et al., 2017).
Tips for Safer Binding
-
Limit Daily Use:
- Aim to bind for fewer than 8 hours per day when possible.
- Take at least one day off each week to allow your body to recover (Peitzmeier et al., 2017).
-
Choose the Right Binder:
- Invest in a well-fitted commercial binder designed for chest compression.
- Avoid improvised methods such as elastic bandages or duct tape, as these can cause severe injuries (Jarrett et al., 2018).
-
Practice Good Hygiene:
- Wash your binder regularly to prevent skin irritation and infections.
- Keep your skin clean and moisturized (Peitzmeier et al., 2017).
-
Listen to Your Body:
- If you experience significant pain, breathing difficulties, or other concerning symptoms, take a break from binding and consult a healthcare provider (Santos et al., 2022).
-
Prepare for Physical Activity:
- Avoid binding during exercise to reduce strain on your chest and lungs (Peitzmeier et al., 2017).
-
Explore Alternatives:
- If binding is causing severe discomfort, consider loose clothing or sports bras as temporary options (Jarrett et al., 2018).
The Role of Healthcare Providers
Healthcare providers play a vital role in supporting individuals who bind. Open and affirming discussions about binding practices and health risks can empower patients to make informed decisions. If you’re experiencing severe symptoms or need advice, seek out gender-affirming care (Peitzmeier et al., 2017).
Looking Ahead
Chest binding is a deeply personal practice that carries both profound benefits and potential risks. While more research is needed to understand its long-term effects, current studies emphasize the importance of safe practices to minimize health complications.
By following the tips above and staying informed, you can enjoy the mental health benefits of binding while protecting your physical well-being.
References
- Peitzmeier, S., Gardner, I., Weinand, J., Corbet, A., & Acevedo, K. (2017). Health impact of chest binding among transgender adults: A community-engaged, cross-sectional study. Culture, Health & Sexuality, 19(1), 64-75. https://doi.org/10.1080/13691058.2016.1191675
- Santos, W. J., Silva, R. B., Rodrigues, D. F., Rocha, L. M. F., & Ceballos, A. G. C. (2022). Chest binding and respiratory complaints in transgender men. Fisioterapia em Movimento, 35, e35107. https://doi.org/10.1590/fm.2022.35107
- Jarrett, B. A., Corbet, A. L., Gardner, I. H., Weinand, J. D., & Peitzmeier, S. M. (2018). Chest binding and care seeking among transmasculine adults: A cross-sectional study. Transgender Health, 3(1), 170-178. https://doi.org/10.1089/trgh.2018.0017